During the early stages of discovery, I conducted nine in-depth interviews with RHC patients to explore their experiences across the entire care journey, from referral and appointment booking to treatment and follow-up. These conversations revealed the emotional and practical challenges patients faced. Instead of relying on assumptions or internal perspectives, I focused entirely on capturing the patient voice to build a picture of their current experience.
I used insights from the nine patient interviews to create one unified care journey map, reflecting common patient experiences. This map identified key pain points and breakdowns, highlighting areas for improvement and aligning the team with real patient needs. Grounded in authentic patient stories, the map helped build a shared understanding, providing a foundation for designing a more compassionate, effective healthcare service.
Mapping the user journey
Uncovering a hierarchy of patient needs
Through interviews with private healthcare users, we identified a clear hierarchy of needs that shaped our design approach.
1. Brilliant basics
At the foundation, patients want an experience that feels fast, smooth, and joined-up. They expect the fundamentals to work flawlessly: quick bookings, short waits, timely responses, consistent communication, and seamless coordination between teams. These are the basics they assume private care will always get right.
2. Trust and control
Emotionally and functionally, trust and control go hand in hand. Patients need to feel they can rely on the service when it comes to something as important as their health. Empathetic communication, personalised care, and being kept informed help build that trust. But choice is just as vital. Letting patients pick appointment times, communication methods, and how they track their care gives them a sense of autonomy and transparency. This reduces anxiety, deepens trust, and makes them active participants in their care.
3. Reassurance as the outcome
Smooth, frictionless progress combined with support at every stage helps patients feel confident they are in safe, capable hands. That reassurance is crucial during a journey often marked by overwhelm, uncertainty, and anxiety.
This hierarchy shaped both what we designed and how we approached every decision, aiming to ease stress, build trust, and support people functionally and emotionally at every step.

I reframe problems as opportunities, and Ramsay was no exception. By analysing the current-state journey map, I identified ten key opportunity areas where the experience broke down, expectations weren’t met, or support was lacking. These insights fueled our ideation sessions, focusing the team on real user needs. As a result, our concepts were more purposeful, clear, and relevant, solving real problems rather than designing abstract solutions.
Creating a seamless, end-to-end service experience

To bring our North Star experience to life, I led a future-state service blueprinting session with multidisciplinary stakeholders from Ramsay, including clinical, operational, digital, and business teams. The goal was to define how our envisioned patient journey would work in practice. I designed and facilitated a day-long workshop to map the experience across frontstage and backstage layers, outlining the roles, processes, technologies, and partners needed to support it.
This collaborative process aligned teams around not just what the experience should feel like, but also how we would deliver it. I refined the blueprint afterward and worked with stakeholders to validate it, ensuring it stayed true to the North Star vision while remaining feasible across the organisation. The result was a practical, strategic tool that now guides delivery planning and cross-team coordination.

Connecting the dots
Turning vision into delivery

Turning pain points into opportunities
Designing the patient journey of the future
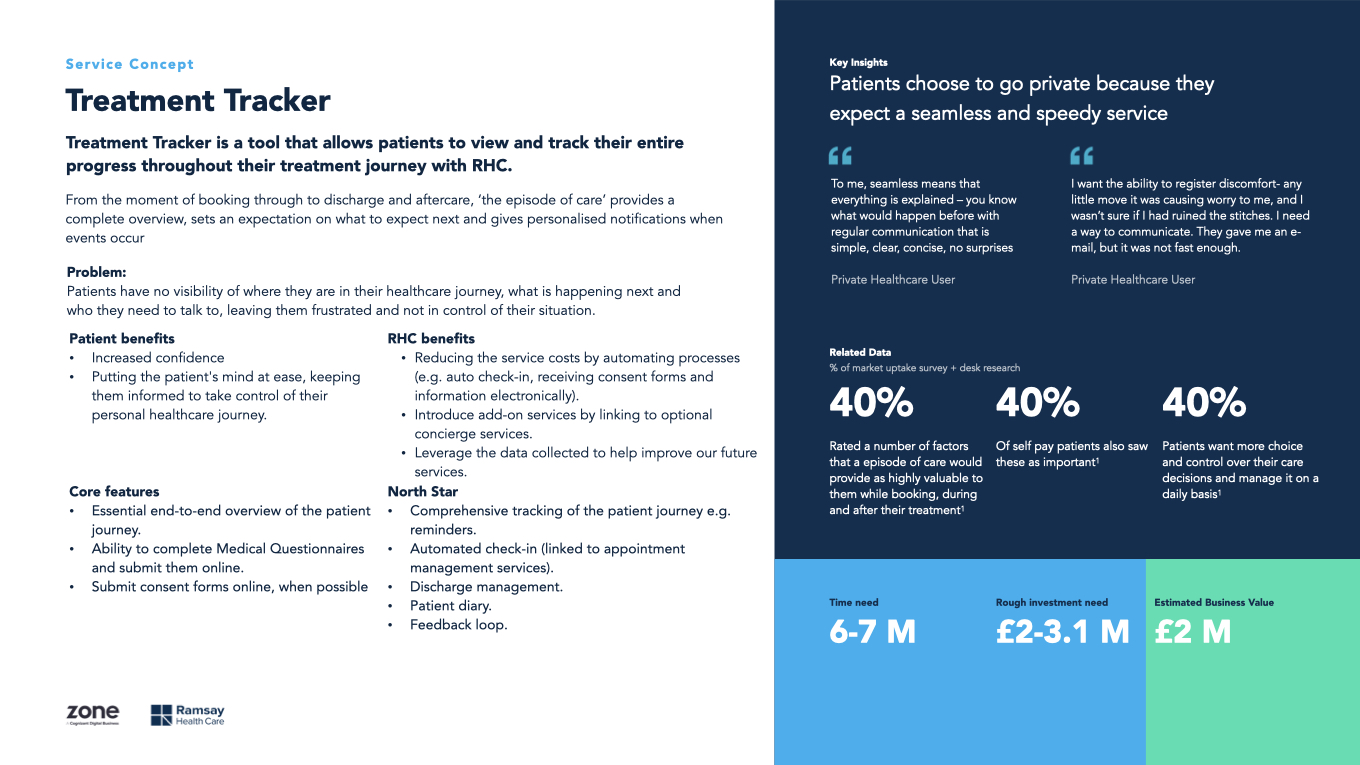
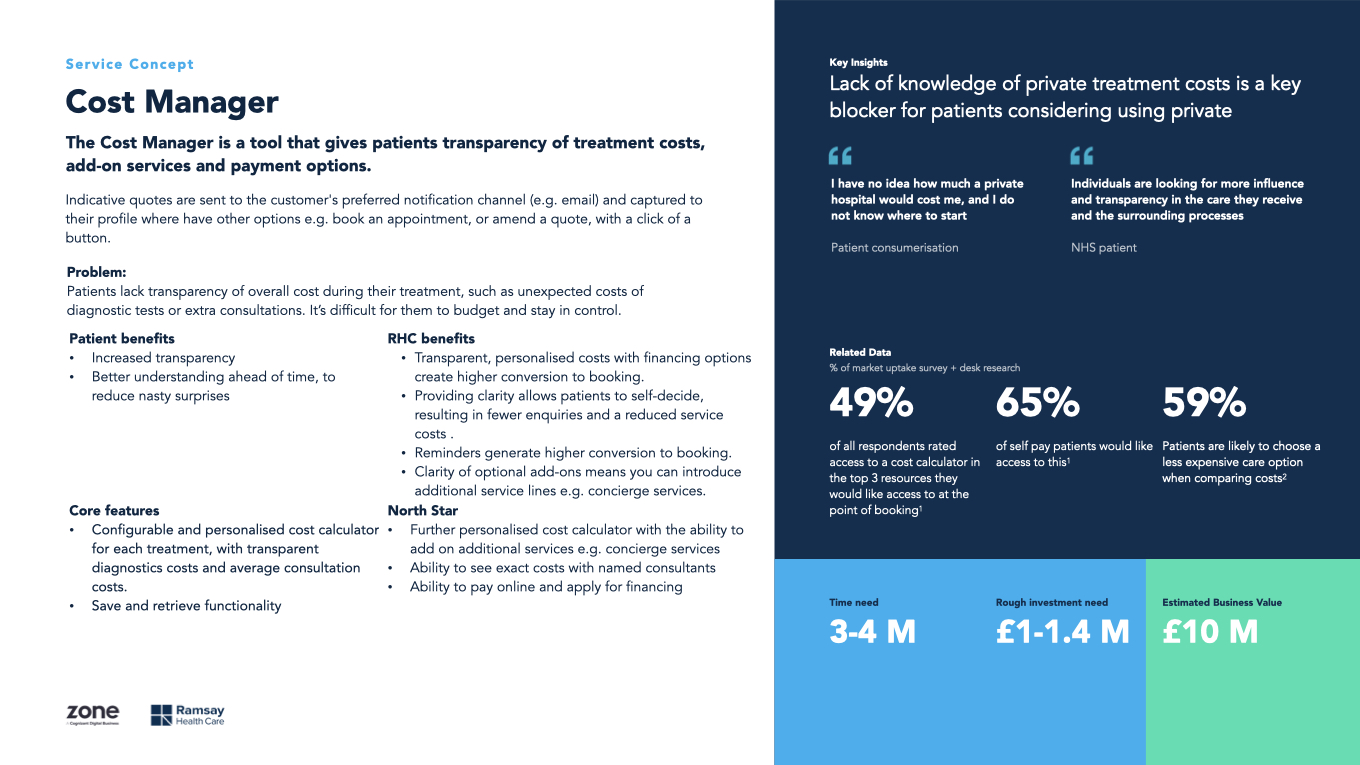
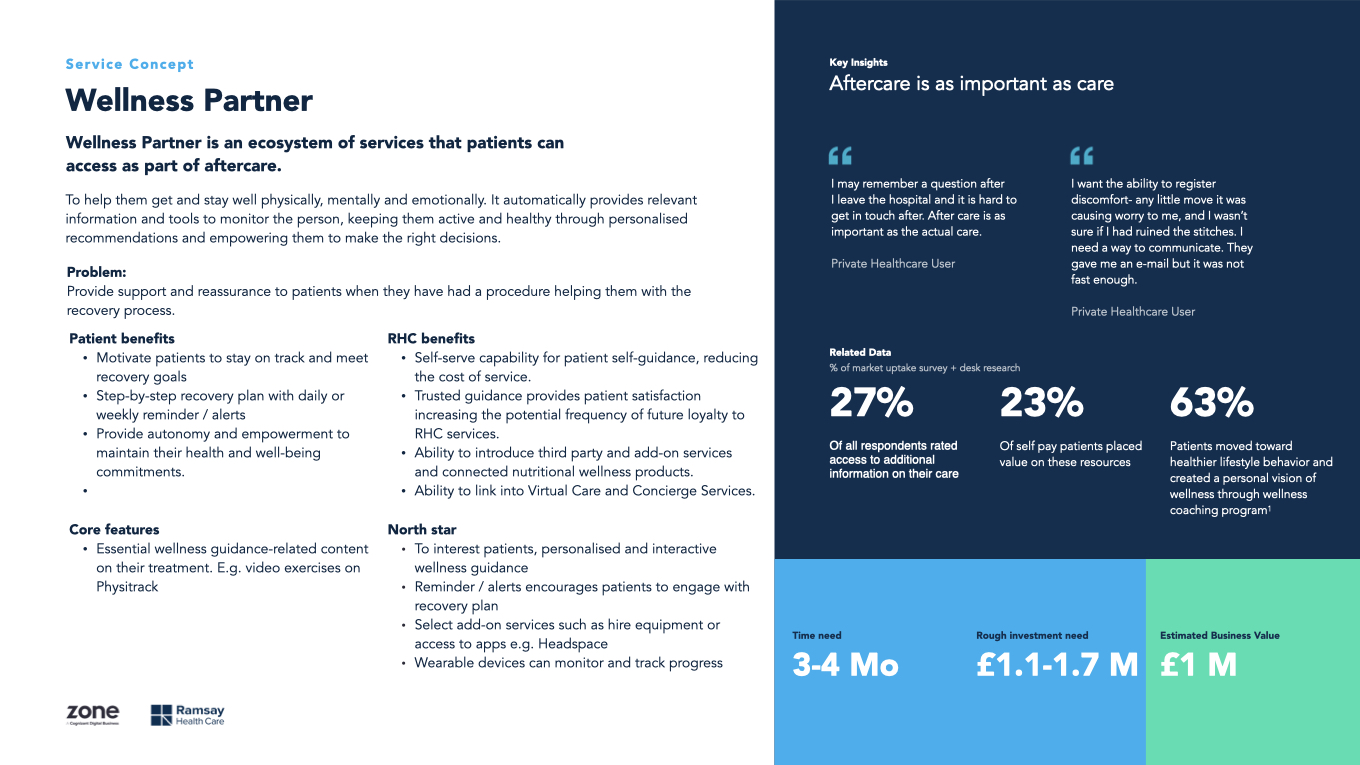
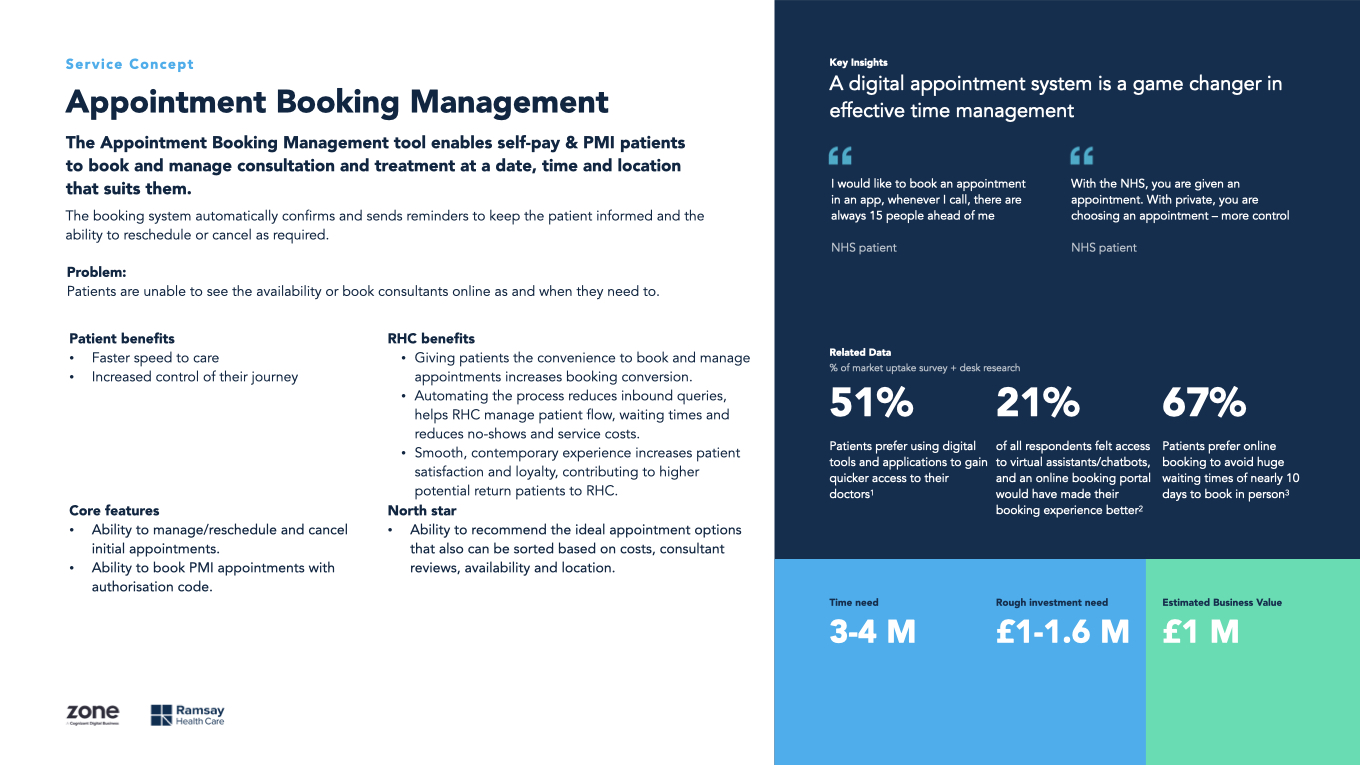
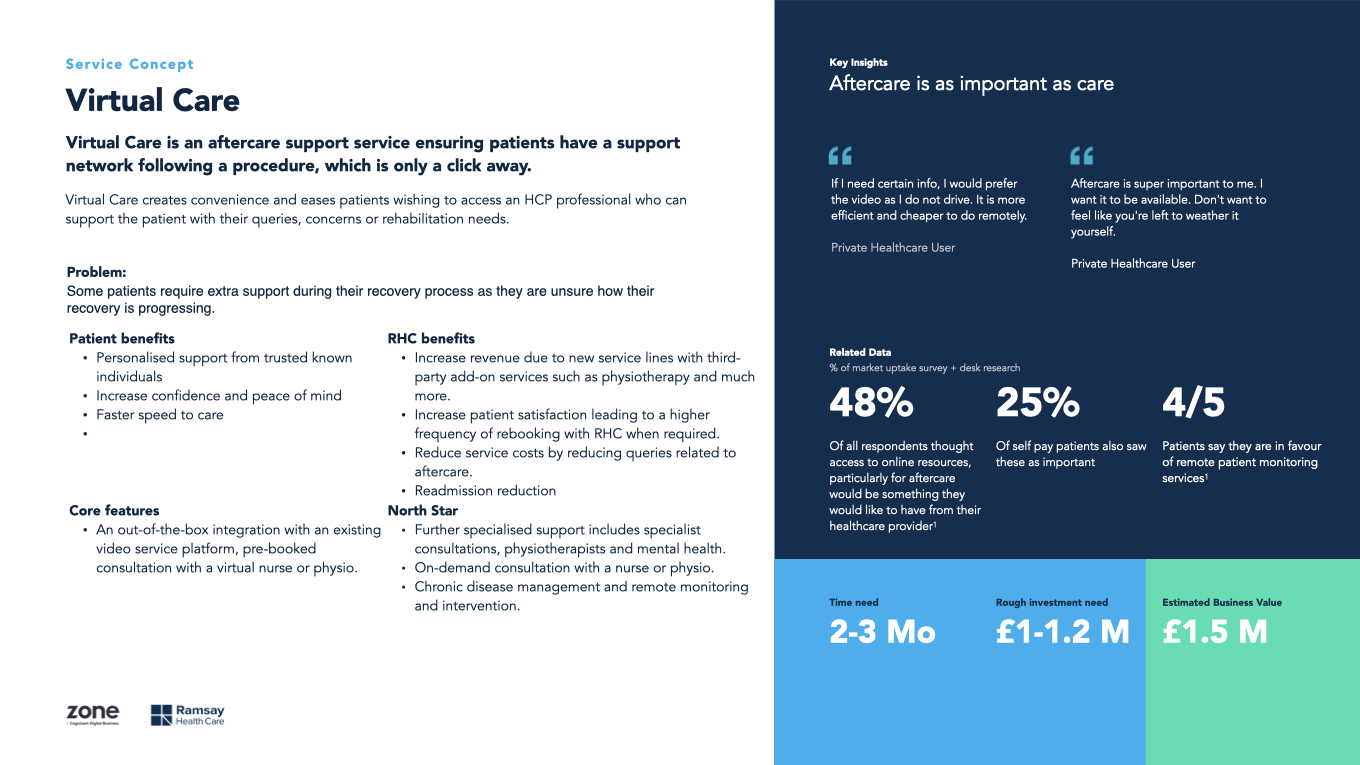
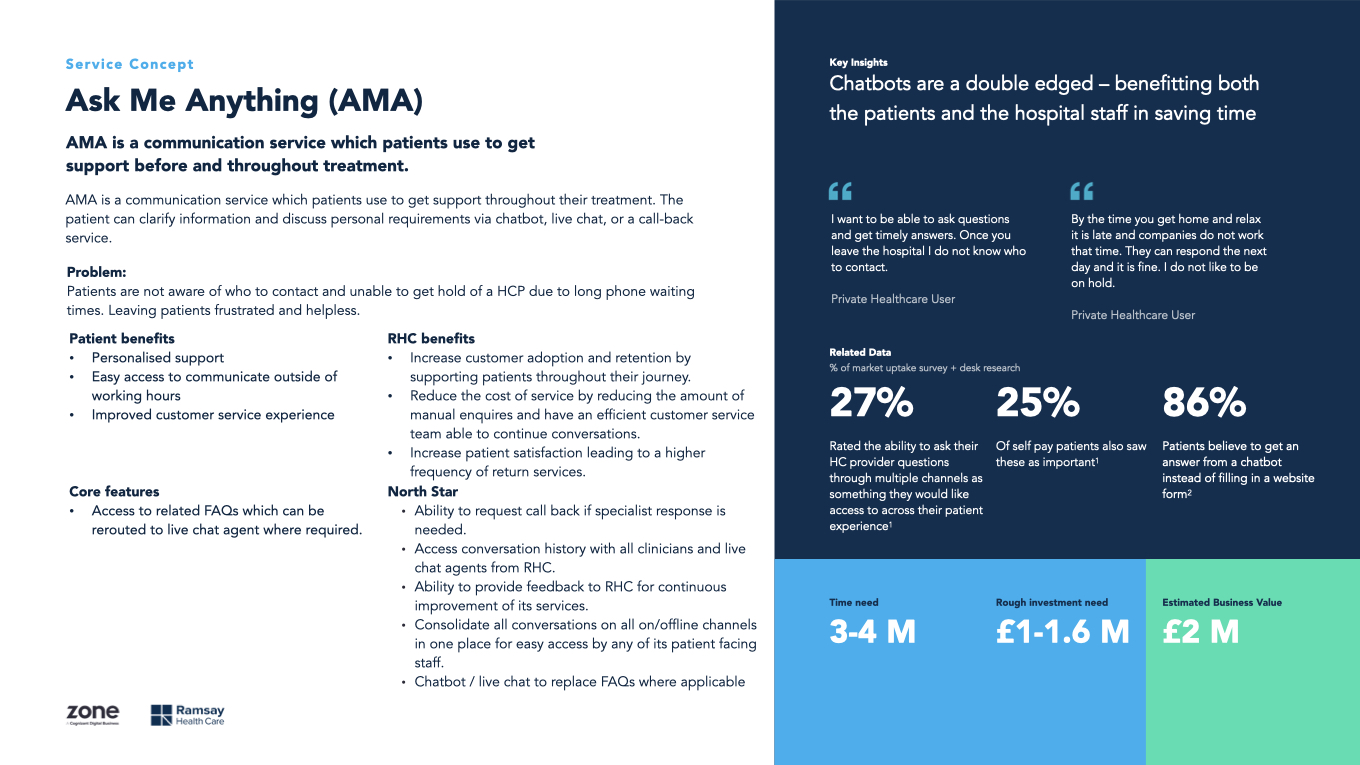
We brought the opportunity areas into a two-day co-creation workshop with Ramsay stakeholders, blending business needs with patient insights. The sessions moved from research playback and value proposition design into fast-paced ideation and prioritisation. Together, we developed nine distinct concepts. Each tackled a key gap in the journey and aligned with Ramsay’s strategic goals. Rather than isolated fixes, these initiatives formed a connected ecosystem that supported patients from first enquiry through to aftercare and delivered improvements across the entire experience.
Our full-service offering is designed to support patients across the entire care journey, with a strong focus on Ramsay’s priority of improving booking conversion. From initial search and profiling, through personalised booking and consultation, to post-treatment support and retention, every feature is mapped to real patient needs and business goals. Value-add initiatives like the Symptom Checker and Wellness Partner enhance the core experience, creating a connected, reassuring journey that builds trust, improves outcomes, and delivers long-term value for both patients and the business.
To bring this full-service vision to life, we needed a clear strategy for phased delivery. It had to prove value early while laying the groundwork for long-term growth. We worked with stakeholders to prioritise initiatives based on business impact and delivery effort, mapping them into a roadmap from MVP to North Star. This helped us align delivery around the features most likely to drive adoption, improve experience, and support long-term outcomes for both patients and Ramsay.